Cardiovascular disease (CVD) remains a leading cause of morbidity and mortality worldwide, prompting continuous research into dietary strategies to mitigate risk. One such dietary factor under investigation is the Glycemic Index (GI) of foods, which measures how quickly carbohydrates in foods raise blood sugar levels. While the benefits of a high-fiber diet are well-documented, the independent role of dietary GI in modulating CVD risk among non-diabetic individuals is less clear. The MEDGI-Carb intervention study aimed to shed light on this issue by examining the effects of low- versus high-GI diets within the framework of a Mediterranean dietary pattern on various cardiometabolic risk factors.
Study Overview
The MEDGI-Carb study was a multinational, randomized controlled trial conducted in Italy, Sweden, and the USA. It involved 160 participants aged between 30 and 69 years, all of whom had a body mass index (BMI) of 25-37 kg/m² and a waist circumference greater than 102 cm for men and 88 cm for women. Additionally, participants exhibited at least one feature of metabolic syndrome, placing them at high risk for cardiovascular disease.
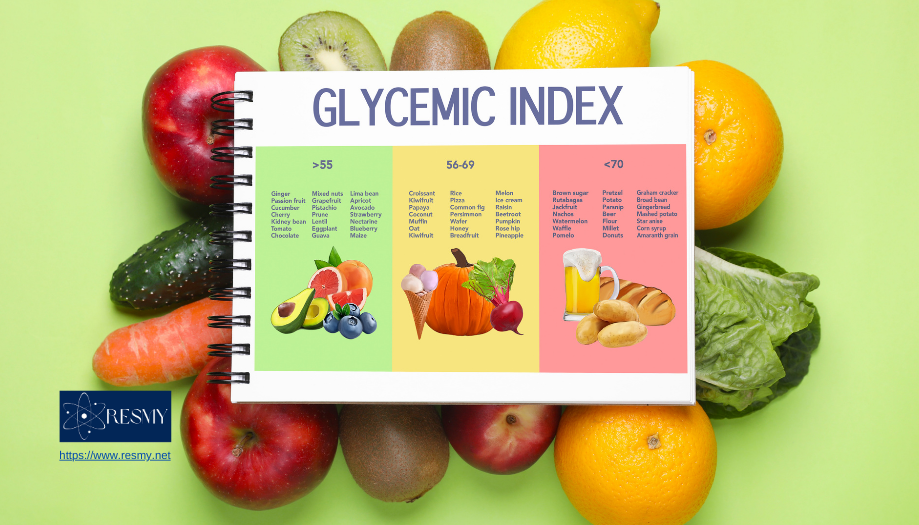
Participants were randomly assigned to follow either a low-GI Mediterranean diet (GI < 55) or a high-GI Mediterranean diet (GI > 70) for 12 weeks. Both diets were designed to be isoenergetic and matched for carbohydrate (270 g/day) and fiber (35 g/day) content to isolate the effects of GI from other dietary components.
Key Findings
- Fasting Metabolic Parameters: At the end of the 12-week intervention, both low-GI and high-GI diet groups showed improvements in several fasting metabolic parameters, including blood pressure, glucose levels, and cholesterol levels. However, no significant differences were observed between the two groups. This suggests that the overall quality and composition of the Mediterranean diet, rather than the GI of individual foods, play a crucial role in enhancing these cardiometabolic markers.
- Postprandial Triglycerides: A notable finding emerged from the subgroup of participants in Italy, where an 8-hour triglyceride profile was measured following standard breakfast and lunch. The low-GI diet significantly reduced the postprandial triglyceride profile compared to the high-GI diet. Although the reduction in plasma triglycerides after lunch (tAUC) was only borderline statistically significant (p = 0.065), the trend suggests a potential benefit of a low-GI diet in managing postprandial lipid responses.
Implications for Cardiovascular Health
The results of the MEDGI-Carb study provide valuable insights into the role of dietary GI in cardiovascular health. While low-GI diets did not show a differential effect on major fasting cardiometabolic risk factors compared to high-GI diets, they did appear to reduce postprandial triglyceride levels. This finding is particularly relevant as elevated postprandial triglycerides are associated with an increased risk of cardiovascular events.
Blood Pressure and Metabolic Parameters: Both diet groups experienced improvements in fasting metabolic parameters, indicating that adherence to a Mediterranean diet, regardless of its GI, can be beneficial for cardiovascular health. This underscores the importance of the Mediterranean diet’s overall nutrient composition, which includes high intake of fruits, vegetables, whole grains, and healthy fats, in reducing CVD risk.
Postprandial Triglycerides: The reduction in postprandial triglycerides observed with the low-GI diet suggests that managing the GI of meals might be particularly useful for individuals who are at high risk of cardiovascular disease due to elevated triglyceride levels. Postprandial hypertriglyceridemia is a known risk factor for atherosclerosis, and strategies to mitigate this can be crucial for improving long-term cardiovascular outcomes.
Study Strengths and Limitations
The MEDGI-Carb study’s strengths include its randomized controlled design, the use of a well-defined Mediterranean diet, and the focus on a high-risk population. Additionally, the multi-national aspect of the study enhances the generalizability of the findings across different populations.
However, some limitations should be noted. The primary analysis did not find significant differences between the low- and high-GI diets for fasting parameters, suggesting that other factors might overshadow the impact of GI in such a dietary pattern. Furthermore, the specific measurement of postprandial triglycerides was limited to the Italian cohort, which might affect the robustness of this particular finding. The borderline statistical significance of the reduction in plasma triglycerides after lunch also warrants further investigation.
Conclusion
The MEDGI-Carb study contributes to the growing body of evidence on the influence of dietary GI on cardiovascular health. While a low-GI Mediterranean diet did not significantly outperform a high-GI Mediterranean diet in terms of fasting metabolic parameters, it showed promise in reducing postprandial triglyceride levels. These findings highlight the potential of incorporating low-GI foods into dietary recommendations for individuals at high risk of cardiovascular disease, particularly for managing postprandial lipid responses.
As cardiovascular disease continues to be a major health concern, further research is needed to fully understand the implications of dietary GI and its integration into comprehensive dietary strategies. In the meantime, promoting a balanced Mediterranean diet, rich in whole foods and low-GI options, remains a viable approach to improving cardiometabolic health and reducing the burden of cardiovascular disease.
Practical Recommendations
For individuals looking to optimize their cardiovascular health, particularly those at high risk of CVD, consider the following dietary tips:
- Choose Low-GI Foods: Incorporate more low-GI foods such as legumes, whole grains, non-starchy vegetables, and most fruits into your diet.
- Follow a Mediterranean Diet: Emphasize a Mediterranean dietary pattern that includes plenty of fruits, vegetables, nuts, seeds, whole grains, and healthy fats like olive oil.
- Monitor Postprandial Triglycerides: If you are at high risk for CVD, consider having your postprandial triglyceride levels checked and discuss dietary adjustments with your healthcare provider.
- Maintain Overall Dietary Quality: Focus on the overall quality and balance of your diet rather than just the GI of individual foods. A nutrient-rich, balanced diet supports overall health and can help reduce the risk of chronic diseases.
By adopting these dietary practices, individuals can take proactive steps towards better cardiovascular health and potentially reduce their risk of developing cardiovascular disease.
Other Topics: Medicine and Health Science, Natural Science, Agricultural Science, Engineering & Technology, Social Sciences & Humanities